Medicaid is the federal medical insurance program for persons who are elderly or disabled. While it is subject to federal legal minimum standards for coverage, the states are given wide latitude to offer additional programs for certain groups and to manage the programs under state regulations and policies. Funding for Medicaid is part federal funds, part state funds. The portion of federal funds is tied to a percentage of the state’s budgeted portion for Medicaid and is called the “federal match rate.” For each dollar a state legislature appropriates for Medicaid, the federal government will contribute between $1 and $3 to that state’s Medicaid budget. Mississippi, as a poorer state, receives $3 for every $1 of state funds, or a 75% match rate. In November 2016 approximately 762,709 adults and children were covered by Medicaid in Mississippi.
Medical costs are a major driver of the inflation rate in the U.S. The Consumer Price Index inflation rate for 2016 is projected to be 1.15% and 1.84% for 2017. https://knoema.com/products/world2020/cpi-inflation-growth Online health care researchers with PwC’s Health Research Institute project the 2017 medical cost trend to be the same as the current year – a 6.5% growth rate, or over three times the general inflation rate. (This rate is down from 9% in 2010, and PwC finds signs that the decade’s slowing medical cost growth rate could tick back up as new healthcare access points (such as retail clinics and urgent care centers) increase utilization of medical services by patients.)
Thus, Mississippi currently receives the maximum amount of federal funds to help provide increasingly expensive medical services to over three-quarters of a million residents. Some lawmakers in Congress have advocated trimming the Medicaid budget by moving away from the current federal match to a “capitated” or “per capita cap” system. The following short article from the National Health Law Program shows how such a change would cut millions of dollars from Mississippi and other states and result in cuts in services to older adults, persons with disabilities, pregnant women and children in poverty, and other vulnerable populations.
What is a Per Capita Cap?
A per capita cap is a financing tool that is being proposed to dramatically cut Medicaid funding. Today, states receive Federal Medicaid funding based on the actual costs of providing services to older adults, persons with disabilities, pregnant women and children in poverty, and others. Under a per capita cap, the Federal government makes a capped payment to the state, and the state does not receive money based on actual costs.
Here’s how it works. Under Medicaid today, for every dollar a state actually spends on Medicaid services, it gets $1 to $3 of Federal support (richer states get $1, poorer states get $3). States are guaranteed continued support for actual costs, even if those costs go up. With a per capita cap, the Federal government makes a limited payment to the state based on a preset formula, which does not increase based on actual costs. Per capita caps have two components which both cause problems.
- In the first year of a per capita cap, Congress would set an initial allotment which is supposed to be based on the expected actual costs. Many per capita cap proposals underestimate this amount, so the state already gets a cut in the first year.
- More importantly, the initial allotment is increased every year by a preset growth index, such as the consumer price index. The problem is, capped payments based on such a growth index increase much slower than actual health care costs. This means that every year the state’s actual costs grow much faster than the federal support.
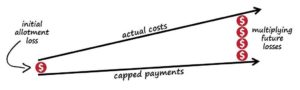
CONCLUSION: Under a per capita cap, the capped payments to states increase much slower than actual costs, leading to large and multiplying losses for states. Over time, states will lose billions of dollars. Per capita caps are a huge federal cost-shift onto states, which will force states to cut Medicaid services for older adults, persons with disabilities, pregnant women and children in poverty, and other vulnerable populations.
By: Leo Cuello , NHeLP, December 13, 2016 http://www.healthlaw.org/component/jsfsubmit/showAttachment?tmpl=raw&id=00Pd000000flqnnEAA
For more questions and concerns on this case, we have the experienced lawyers at Courtney Elder Law to assist you. Contact us today by calling 601-987-3000.
